STILLBIRTH(syn. stillbirth) - the birth or removal of a fetus from the mother’s body during pregnancy from 28 weeks. or more, i.e. a fetus with a height of 35 cm or more, weighing 1000 g or more, which, after separation from the mother’s body, did not take a single breath. The statistical indicator M. is calculated as follows:
([number of children stillborn] / [number of children born in total (living and dead)]) x 1000
In this case, a fetus is considered stillborn if it does not have independent extrauterine pulmonary respiration at birth and if resuscitation by artificial means is unsuccessful, regardless of the presence of a heartbeat or other signs of life.
The rate of stillbirths of full-term and premature infants (to the number of all full-term or premature infants) is calculated similarly. According to G.F. Tserkovny (1976), antenatally dead fetuses account for about 40% of all stillborns; premature babies are 7-8 times more likely to be stillborn compared to full-term babies. According to V.I. Grishchenko and A.F. Yakovtsov (1978), the level of M. indicator in individual countries ranges from 5 to 20 ppm, including in developed countries M. indicators are the lowest.
Depending on the timing of death in relation to childbirth, M. is divided into antenatal and intranatal. M. is considered antenatal in cases where fetal death occurred within 28 weeks. and before childbirth; antenatal death of the fetus is established on the basis of a wedge (cessation of heartbeat and fetal movements before the onset of labor) and rentgenol, signs. M. is considered intranatal in cases where death occurred during childbirth; Newborns born with a heartbeat, but who did not begin to breathe after resuscitation measures, should also be included as intrapartum deaths.
Causes of stillbirth
The causes of stillbirth are varied and not fully studied: patol, processes in the mother’s body, the fetus itself and the so-called. fertilized egg. The pathology of the fetus and changes in the placenta largely depend on previous and concomitant diseases of the mother, complications of pregnancy and childbirth. The causes of ante- and intrapartum stillbirth can be divided into main and immediate. The main causes of M. are: complications of pregnancy (late toxicosis, bleeding, etc.), anomalies of labor, fetal position and placenta previa, pathology of the umbilical cord and placenta, maternal diseases not related to pregnancy: heart defects, hypertension, nephropathy, diabetes , acute and chronic. inf. diseases, acute poisoning, immunol, incompatibility of mother and fetus, etc. The immediate causes of antenatal fetal death can be asphyxia, hemolytic disease, intrauterine infection, congenital malformations and genetic diseases. Intranatally, the fetus may die due to pathol, during labor (intracranial birth trauma, fetal asphyxia, maternal eclampsia, placenta previa, etc.).
The pathological examination aims to find out the cause of fetal death: fetal asphyxia, birth trauma, and whether the fetus was viable or whether there were malformations incompatible with life or intrauterine disease. In each specific case of asphyxia or birth trauma of the fetus, it is necessary to establish whether these conditions were the main cause of death or a complication of a previous intrauterine disease of the fetus - Fetopathy (see). Macroscopic signs of a stillborn fetus that died antenatally are, as a rule, severe maceration of the skin, autolysis of internal organs, lack of air in the stomach and complete primary atelectasis of the lungs. As a result of maceration, the epidermis of the fetus falls off in layers in the form of grayish-white films, revealing a moist bluish-red dermis; the internal organs are flabby, spread apart when cut, and there is a greater or lesser amount of clear bloody fluid in the body cavities. Autolysis of internal organs makes microscopic examination difficult. The lungs are preserved longer than other organs, which must always be subjected to microscopic examination. Maceration of the skin and autolysis of internal organs are more pronounced the longer the dead fetus was in utero; if the fruit was extracted quickly, maceration and autolysis may not occur.
The placenta, due to the cessation of fetal circulation and the preservation of maternal blood circulation, is anemic as a result of compression of the vessels of the villi.
The stomach of a stillborn does not contain air and has collapsed; the lungs are pressed to the root, do not fill the chest cavity, are fleshy, bluish-red, and dark liquid blood appears on the cut surface when pressed. Hydrostatic vital tests (see) negative. It is imperative to take into account the presence of air pockets in the lungs resulting from artificial respiration during resuscitation; Microscopically, artificial air areas differ from the natural expansion of the lungs by the presence of large air cavities with ruptures of the alveolar septa (Fig. 1), interspersed with areas of atelectasis (see).

In the absence or insignificant severity of maceration and autolysis, it is possible to identify signs of fetal disease in the organs, characteristic of fetopathies of any etiology. These include an increase or decrease in the total weight of the fetus that does not correspond to its age, the presence of dystrophic and focal necrotic changes in parenchymal organs, hepato- and splenomegaly with the presence of large foci of myeloerythropoiesis that do not correspond (in size) to the age of the fetus, interstitial infiltrates mainly from eosinophilic myelocytes in the liver, pancreas and thymus gland, accidental involution with a decrease in the mass of the thymus gland, the presence of immaturity and malformations of tissues, for example, cystic dysplasia of the kidneys (Fig. 2). In addition to these general signs, changes are observed that are characteristic, for example, of isoimmune hemolytic disease of the fetus, congenital listeriosis, syphilis, toxoplasmosis, cytomegaly, mycoplasmosis, rubella, chickenpox, serum hepatitis, diabetes, thyrotoxicosis, and certain congenital diseases.
Due to the fact that many diseases of a stillborn fetus are not macroscopically recognized, it is necessary to comprehensively apply microscopic, bacterial, cytogenetic, immunofluorescent and biochemical. methods for studying organs and placenta.
X-ray diagnostics
The need for X-ray diagnostics may arise before the pathological and forensic medical examination. autopsy of the fetal corpse, as well as in the case of a wedge, signs of intrauterine death of the fetus. The reason for rentgenol, research may be certain difficulties in differentiating live birth and stillbirth during a sectional study, the need to compare the results of hydrostatic vital tests with the results of rentgenol, research, as well as cases of pronounced cadaveric decomposition.
So-called Dillon's test, which consists of detecting signs of gas in the digestive tract of a corpse on an x-ray (according to the scientist, this indicates live birth), cannot be considered as a reliable indicator. According to many researchers, such a rentgenol study loses its diagnostic value after 48 hours. after death due to the development of putrefactive processes in the gastrointestinal tract. tract and in cases of artificial respiration.
With X-ray The study should obtain an image of the entire corpse, and, if necessary, individual organs. Radiographs are taken in frontal and lateral, and sometimes in additional targeted projections.

Basic rentgenol, signs of stillbirth: 1) complete absence of gas in the lungs, stomach and intestines (Fig. 3, a); 2) absence of gas in the lungs, however, the presence of gas in the digestive tract is possible, but not further than the duodenum (Fig. 3, b); 3) slight expansion of the lungs is possible in the complete absence of gas in the stomach and intestines; 4) the presence of gas in the cavities of the heart and large vessels (Fig. 3, b). These signs exclude a live birth.
A certain similarity with the above-listed rentgenol signs can be observed in a live birth in the absence of lung expansion in combination with the presence of gas in the intestines; however, the gas occupies the small intestine over a large area - beyond the duodenum, which indicates an undoubted live birth of the child even with complete airlessness of the lungs. The possibility of a newborn's life for several hours with complete non-expansion of the lungs is explained by the fact that the gas contains gas. tract diffuses a certain amount of oxygen. As A. Ilyine’s research has shown, even 5% of the normal amount of oxygen necessary for life can temporarily support the life of a newborn at rest.
Despite the relative diagnostic value of rentgenol, research, it in combination with other methods is of undoubted importance for forensic medicine. examination.
Stillbirth in forensic terms
Establishing the fact of stillbirth is important in the investigation of criminal cases related to infanticide (see) during childbirth outside of medicine. institutions.
When examining a corpse, attention is paid to the presence of external signs of pulmonary respiration: the shape of the chest in stillborns is less convex than in liveborns, the level of the dome of the diaphragm in stillborns corresponds to the IV, in liveborns - to the VI rib (however, these signs are inconsistent and unreliable). The volume and color of the lungs are of diagnostic importance: the lungs of a stillborn are not expanded, collapsed, as a rule, they are located in the posterior parts of the chest cavity; Their color is reddish-brown or brownish-red, their lungs are dense and elastic to the touch. To determine stillbirth. or live birth, it is necessary to conduct two vital hydrostatic (swimming) tests - pulmonary and gastrointestinal, based on determining the presence of air in the lungs and gastrointestinal tract. tract (see Vital tests).
Gistol, the study of the lungs of a corpse, is of great diagnostic importance. A stillborn is characterized by: unstraightened alveoli and bronchi, a cubic shape of the alveolar epithelium, thick interalveolar septa, convoluted elastic fibers running in less thick bundles, thin convoluted argyrophilic fibers. Other organs and tissues of the corpse are also examined, for example, the umbilical ring, umbilical cord.
For the differential diagnosis of stillbirth and live birth, I. K. Esipova, O. Ya. Kaufman (1968) developed a method of post-mortem X-ray vasography in combination with micrometry of the arteries at the level of the respiratory bronchioles, the weight ratios of the parts of the heart, the condition of the umbilical vessels and the arterial (botallian) duct. In stillborns, radiographs reveal varying degrees of filling of the vessels with the contrast mass. The lumen of the arteries at the level of the respiratory bronchioles of stillborns is 0.2±0.54 µm. In live births, the intralobular arteries of the lungs form an extremely dense network, merging in places. The lumen of the arteries at the level of the respiratory bronchioles in live births by the second day of life is 18-20 microns. However, the introduction of a contrast agent into the pulmonary trunk or into the aorta of a corpse makes swimming tests impossible.
In connection with the cessation of blood flow through the umbilical vessels, and later through the ductus arteriosus, the beginning of the organization of blood clots in the umbilical vessels and cell proliferation in the subendothelial layer of the ductus arteriosus is of diagnostic importance. The development of these processes begins quite early and serves as evidence of viviparity.
In expert practice, it is often necessary to examine the corpses of newborns not only soon after death, but also after various periods, when putrefactive changes and drying out occur. In these cases, the evaluation of the results of the tests described above must be approached with caution. When examining stillbirths, especially in cases of putrefactive changes or drying out of corpses, the method of emission spectral analysis of the lungs, liver, blood, myocardium and placenta is used (see Spectral analysis). In spectrographic studies, coefficient values are used in the ratio of certain macro- and microelements. It is advisable to use the lab complex. methods, which reduces the number of expert errors.
Prevention of stillbirth
Prevention of stillbirth includes a set of health-improving measures (gymnastics, walks, good nutrition for the pregnant woman, adherence to a work-rest regime, etc.), especially with a burdened obstetric history (fetal death in the past), with diseases of the woman that can subsequently cause fetal death during pregnancy (sugar diabetes, heart defects, hypertension, diseases of the genital organs, Toxoplasmosis, etc.), as well as in antenatal pathology (see). If possible, conduct a medical genetic consultation (see). Pregnant women with one or another pathology are sent to a specialized hospital to monitor the condition of the pregnant woman and fetus and appropriate treatment to prevent spontaneous abortion or death of a viable fetus (see Antenatal fetal care).
Bibliography: Burov S. A. and Reznikov B. D. Radiology in forensic medicine, p. 206, Saratov, 1975; Grishchenko V.I. and Yakovleva A.D. Antenatal fetal death, M., 1978, bibliogr.; D and l-l about n Ya. G. X-ray vital test and its rationale, Vestn, rentgenol., t. 23, No. 2, p. 91, 1939; Potter E. Pathological anatomy of fetuses, newborns and young children, trans. from English, M., 1971, bibliogr.; Tserkovny G. F., F r o l o v a O. G. and K o b o - z e v a N. V. About statistical criteria of the perinatal period, Obstetrics, and gynec., Jvft 3, p. 24, 1976; Ellenbogen L. S., Bayer H. a. G o t t 1 i e b M. Roentgen demonstration of gas in the fetal circulatory system, a valuable sign of fetal death, Radiology, v. 67, p. 410, 1956; Gruber G. H. Gas in the umbilical vessels as a sign of fetal death, ibid., v. 89, p. 881, 1967; Y 1 p o 6 A. Uber Magenatmung beirn Men-schen, Biochem. Z., Bd 78, S. 273, 1917.
O. G. Frolova; T. E. Ivanovskaya (pat. an.), G. A. Pashinyan, P. P. Shirinekiy (court), S. A. Sviridov (rent.).
Live birth rate is the complete expulsion or removal of the product of conception from the mother's body, regardless of the duration of pregnancy, which after such separation breathes or shows other signs of life, such as heartbeat, muscle contraction, pulsation of the umbilical cord, regardless of whether it is cut or not, placenta detached. Each product of such a birth is considered a live birth.
Fetal death (stillborn fetus) is the death of the product of conception before it is completely expelled or removed from the mother’s body, regardless of the duration of pregnancy. Death is indicated by the fact that after such separation the fetus does not breathe or show any other signs of life, such as heartbeat, pulsation of the umbilical cord or certain muscle movements.
Full term newborn- a child born at a gestational age of 37 weeks to 42 weeks with average body weight. In a full-term newborn baby, the head makes up 1/4 of the body. Determining head shape and skull circumference at birth is important . During the first 2-3 days of life, the child retains the configuration of the skull, which is caused by the passage of the head through the mother’s birth canal. Normal variants include skull shapes such as dolichocephalic, brachycephalic, and tower-shaped skulls. The head circumference in full-term babies is 33-36 cm, and may exceed the chest circumference by 1-2 cm. The large crown is open, its size normally does not exceed 2.5-3 cm. The small crown is no more than 0.5 in diameter cm - can be open in 25-30% of full-term newborns.
Premature newborn- a child born between 24 and 37 completed weeks of gestation.
Post-term newborn- a child born at 42 completed weeks of gestation or more.
When comparing indicators of the child’s physical development and gestational age(gestational age) the following groups of children are distinguished:
1. Newborns with large body weight.
2. Newborns with normal physical development for a certain gestational age.
3. Newborns with low body weight for gestational age or newborns with intrauterine growth retardation.
4. Newborns with intrauterine (congenital) malnutrition.
Prevention of stillbirths largely consists of protecting the woman’s health, especially during pregnancy (see Antenatal fetal care) and careful management of normal and pathological labor.
Stillbirth is the birth after 28 weeks of intrauterine life of a fetus with a length of at least 35 cm and a weight of at least 1000 g, which has not taken a single breath at birth. Stillborns are also considered children who were born with a heartbeat, but did not take a single breath, despite the measures taken to revive them (fetuses born with asphyxia and not revived).
A distinction is made between antenatal and intranatal fetal death. Antenatally dead include fetuses whose intrauterine death occurred between 28 weeks before birth. Intranatal death is considered to be the death of a fetus that occurs during childbirth.
The causes of stillbirth are varied and not yet fully understood. Stillbirth is caused by pathological processes occurring in the mother’s body, the fetus itself and in the fertilized egg.
The pathology of the fetus and changes in the placenta largely depend on the diseases of the mother, complications of pregnancy and childbirth.
In the pathogenesis of ante- and intranatal fetal death, the main role is played by asphyxia (see), which can occur with maternal diseases of a wide variety of nature and complications of pregnancy and childbirth. Infections (acute - influenza, typhoid, pneumonia, etc.; chronic - malaria, syphilis), intoxications (acute poisoning, toxicosis of pregnancy), hyperthermia, etc. are important. In the pathological course of labor, cerebral circulation disorders of the fetus and the so-called intracranial birth injuries.
The combination of asphyxia and birth trauma is especially dangerous.
Etiology. In the antenatal period, the fetus may die due to infectious (and viral) and severe systemic diseases of the mother (heart defects, hypertension, nephropathy, diabetes, etc.), toxicosis of the second half of pregnancy, immunological incompatibility between the body of the mother and the fetus, as well as due to abnormalities in the development of the fetus, placenta and umbilical cord, with placenta previa, prenatal rupture of water and other pathological processes (see Intrauterine death).
Among the causes of intrapartum fetal death, a significant role is played by complications of childbirth with a narrow pelvis, anomalies of labor forces, incorrect positions (transverse, oblique) and various deviations from the normal mechanism of labor (incorrect insertion of the head, complications of childbirth in the breech presentation and some pathological processes). Fetal death during childbirth often occurs with placenta previa, uterine rupture, eclampsia, etc.
Pathological diagnosis. With antenatal death, maceration of the skin is observed in 90% of cases. Since maceration also occurs in live births (although very rarely and in limited areas), only severe maceration is a sign of stillbirth. Due to the cessation of fetal circulation and the preservation of maternal blood circulation, the placenta becomes anemic as a result of compression of the vessels of the villi.
The most common causes of fetal death are: intrauterine asphyxia caused by pathology of the placenta (premature abruption, malformations, large infarctions, blood clots, hemangiomas), umbilical cord (true nodes, torsion, shortness); maternal illnesses accompanied by anoxemia; less often - infectious diseases of the fetus (intrauterine pneumonia with early discharge of water, listeriosis); fetal malformations or hemolytic disease occurring without jaundice. Negative hydrostatic tests are of great diagnostic value (see Live birth). The lungs of the fetus are usually fleshy and pressed towards the root; less often they are completely expanded, but contain not air, but amniotic fluid.
In intrapartum death, fetal maceration and placental ischemia are usually absent. Hydrostatic tests are negative, but during artificial respiration they can be positive. The most common causes of death are: asphyxia, birth trauma of the skull (ruptures of the tentorium, falx, subdural hemorrhages, rarely fractures of the skull bones) with anomalies in the position and presentation of the fetus, early discharge of water, discrepancy between the sizes of the fetal head and maternal pelvis; rapid birth. Birth trauma of the spine (its stretching with epi-, intra- or subdural or subarachnoid hemorrhages, less often with hematomyelia or ruptures) is observed less frequently, more often with traction of the fetus by the pelvic end. Trauma to the premature fetus is also possible during normal birth. Fetal asphyxia occurs as a result of placenta previa or abruption, entanglement, nodulation, stretching, compression or prolapse of the umbilical cord, early breaking of waters, and prolonged labor.
The presence of hyaline membranes (see), as a rule, excludes stillbirth.
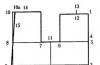
X-ray diagnosis of stillbirth is mainly of forensic interest during the autopsy of a newborn. Previously, sectional recognition of stillbirth was based on the absence of signs of extrauterine respiration, i.e., the absence of air in the lungs. The initial hopes of researchers for the possibility of judging the stillbirth of a fetus only from the X-ray picture of its airless lungs were not justified, since in forensic medical practice there are known cases of complete airlessness of the lungs in undoubtedly live-born people who lived for several hours. However, an X-ray examination of the corpse of a newborn confirms with great accuracy the data of the pulmonary hydrostatic (swimming) test and in this regard is important as an objective control method. But X-ray diagnostics of the state of the respiratory tract alone could not always be sufficient to answer the question of whether a child was born alive or dead, when his lungs turned out to be completely airless. Therefore, X-ray diagnostics when examining the corpses of stillborns and children who died from asphyxia should consist of examining the entire corpse; Particular attention should be paid to the cardiovascular system. In many stillborns, gas is detected in the cavities of the heart and in large vessels. This sign makes it possible to confirm the stillbirth of the fetus with the greatest confidence. During sectioning, these gas accumulations usually do not open. If the presence of a large gas bubble in the heart can be detected sectionally by autopsying the corpse of a newborn under water (which is usually not done, since there are no preliminary indications), then it is impossible to establish gases in the vessels in this way; radiographically they are detected without any difficulty (Fig. 1-4).
X-ray diagnosis of stillbirth: 1 - bell-shaped chest of a stillborn fetus; 2 - gas in the cavities of the heart and blood vessels in a stillborn fetus in the presence of gas in the stomach (direct projection); 3 - the same case in lateral projection; 4 - putrefactive decomposition of the corpse of a stillborn two weeks after birth: a large accumulation of putrefactive gases in the subcutaneous tissue and in the cardiovascular system in the absence of them in the lungs; in the stomach there is a relatively small gas bubble.
Prevention of stillbirth. A pregnant woman is prescribed a diet appropriate to her condition and stage of pregnancy. A thorough examination of the pregnant woman is carried out, including serological examination (Wassermann reaction, determination of the Rh factor, detection of toxoplasmosis). If a disease is detected, timely implementation of therapeutic measures, early hospitalization of pregnant women with abnormal fetal position, breech presentation, multiple pregnancy, polyhydramnios, and with Rh-negative blood factor.
Ministry of Health of the Russian Federation and State Statistics Committee of the Russian Federation
Instructions
on determining the criteria for live birth, stillbirth, and the perinatal period
For the purpose of international comparability of domestic statistics in the field of perinatology and in connection with the transition to the criteria of live birth and stillbirth adopted by the World Health Organization, health authorities and institutions should adhere to the following definitions and concepts of live birth, stillbirth, the perinatal period and parameters of the physical development of the newborn (fetus).
1. Live birth
A live birth is the complete expulsion or removal of the product of conception from the mother's body, regardless of the duration of pregnancy, and the fetus after such separation breathes or shows other signs of life, such as heartbeat, pulsation of the umbilical cord or voluntary muscle movements, regardless of whether the umbilical cord is cut or separated placenta. Each product of such a birth is considered to be a live birth.
2. Stillbirth
Stillbirth is the death of a product of conception before it is completely expelled or removed from the mother's body, regardless of the duration of pregnancy. Death is indicated by the absence of breathing in the fetus after such separation or any other signs of life, such as heartbeat, pulsation of the umbilical cord or voluntary muscle movements.
3. Birth weight
Birth weight is the result of the first weighing of the fetus or newborn, recorded after birth. This weight should be established preferably within the first hour of life before significant weight loss occurs in the postnatal period. Measuring the length of a newborn (fetus) must be carried out in an extended position on a horizontal stadiometer.
Newborns (fetuses) born weighing less than 2500 g are considered low birth weight fetuses; up to 1500 - from very low; up to 1000 g - with extremely low.
4. Perinatal period
The perinatal period begins at 28 weeks of pregnancy, includes the period of childbirth and ends after 7 full days of life of the newborn.
5. Health care institutions register in the medical documentation all those born alive and stillborn, having a birth weight of 500 g or more, regardless of the presence of signs of life, in the manner established by order of the Ministry of Health of the USSR 06.12.86 N 848 pp. 1, ( appendix 2 and 3).
6. The following are subject to registration with the civil registry office:
Born alive or dead with a body weight of 1000 g or more (or, if the birth weight is unknown, a body length of 35 cm or more or a gestation period of 28 weeks or more), including newborns with a body weight of less than 1000 g - in case of multiple births;
All newborns born with a body weight from 500 to 999 g are also subject to registration with the civil registry office in cases where they lived more than 168 hours after birth (7 days).
For each case of death in the perinatal period, a “Perinatal Death Certificate” is filled out. Fetuses born with a body weight of 500 grams or more are subject to pathological examination.
Registration of stillbirths and deaths of newborns in the perinatal period in the civil registry office is carried out by those institutions that issue a perinatal death certificate in the manner established by order of the USSR Ministry of Health N 1300 of November 19, 1984.
7. For the purpose of international comparability of domestic statistics, when calculating the perinatal mortality rate, the number of fetuses and newborns with a body weight of 1000 g or more (or, if birth weight is unknown, a body length of 35 cm or more or a gestational age of 28 weeks or more) is used.
Industry statistics of perinatal mortality, in accordance with WHO recommendations, include all cases of birth of a fetus and newborn with a body weight of 500 g or more (or, if birth weight is unknown, a body length of 25 cm or more or a gestational age of 22 weeks or more ).
Signs of a live birth are:
spontaneous breathing
heartbeat
umbilical cord pulsation
voluntary active movements
If at least one sign is present, he needs to perform resuscitation measures.
Sp iri diseases of newborns: purulent-inflammatory diseases of newborns.
Vesiculopustulosis – one of the most common forms of local infection. This is a pustular disease that can begin in newborns in the first months of life.
Clinical manifestations:
in the natural folds of the skin, on the torso, scalp, and limbs, small superficial blisters appear, initially filled with transparent and then cloudy purulent contents
bubbles open, forming erosions, becoming crusted
the child’s general condition does not suffer.
Prognosis: may be complicated by the development of infiltrates and multiple abscesses.
Pemphigus – is a type of pyoderma. Occurs 3-5 days after birth.
Clinical manifestations:
suddenly, multiple round and oval blisters (up to several centimeters in diameter), single-chamber, with serous fluid that becomes cloudy, appear on the unchanged skin. The walls are thin and easily open, forming erosion.
Most often localized on the back, abdomen, axillary and inguinal skin folds
The rash occurs in bursts, so the rash is polymorphic in nature.
The child's condition is serious, intoxication is severe, the temperature is 39 degrees, the child is lethargic, refuses to breastfeed, and is not gaining weight well.
Prognosis: with timely treatment, recovery occurs in 2-3 weeks, however, if the course is unfavorable, the disease can end in sepsis.
EXFOLIATIVE DERMATITIS – the most severe form of staphylococcal skin lesions of a newborn.
Clinical manifestations:
Diffuse hyperemia appears around the navel or mouth, after some time the epidermis detaches, revealing large erosive areas, the affected area gradually increases, and after 8-12 days the newborn’s skin takes on the appearance of being burned.
The condition is severe, symptoms of intoxication are pronounced, there is a high fever, the child is lethargic, refuses to breastfeed
Abscesses and phlegmon are often associated.
Pseudofurunculosis – inflammation of the sweat glands.
The disease can begin with prickly heat, vesiculopustulosis. The most favorite localization is the skin of the scalp, the back of the neck, the skin of the back, buttocks, and limbs.
Clinical manifestations:
In place of the excretory ducts of the sweat glands, red subcutaneous compactions appear, then purulent contents appear in the center of the inflammatory focus, and after healing a scar remains.
The child’s condition is disturbed, symptoms of intoxication, body temperature periodically rises
Enlarged regional lymph nodes
The disease progresses over a long period of time and in waves.
Prognosis: with timely treatment, recovery occurs in 2-3 weeks; if untimely treatment, it can result in sepsis.
Cellulitis of newborns - one of the most severe purulent-inflammatory diseases, which is an inflammatory process of subcutaneous fat tissue with the subsequent development of necrosis.
The inflammatory process is most often localized on the chest, abdomen, and sacro-gluteal region.
Clinical manifestations:
First, limited redness appears on the skin, dense to the touch, which then quickly increases in size, swelling increases, and has a bright purple color.
It gradually becomes anesthetized, thinning and detachment of the skin occurs, and after its rejection large defects with undermined edges and purulent pockets are formed, the process can spread to deeper tissues, the skin over the affected area becomes black
The child's condition is very serious, symptoms of intoxication, high fever, vomiting, dyspepsia, sleep disturbances, and appetite.
Prognosis: leads to the development of sepsis.
Purulent omphalitis – an inflammatory process in the tissue around the umbilical ring and severe symptoms of intoxication.
Purulent omphalitis can begin with symptoms of catarrhal omphalitis.
Clinical manifestations:
The skin around the navel is hyperemic, edematous, and the venous network on the anterior abdominal wall is dilated.
The umbilical wound is an ulcer covered with fibrin plaque; when pressed, purulent plaque is released.
Gradually, the umbilical area begins to bulge, deep tissues become involved
Umbilical vessels are inflamed
The child's condition is serious, symptoms of intoxication are pronounced, he is lethargic, sucks poorly, has a high temperature, and is not gaining weight.
Prognosis: with timely treatment, recovery occurs in 2-3 weeks, but may be complicated by sepsis.
Sepsis is a severe infectious disease characterized by a generalized course of inflammatory processes that occurs as a result of the penetration of pathogenic microbes and their toxins into the blood, against the background of reduced immunity of the body.
Risk factors for developing sepsis:
massiveness and virulence of infection
immunodeficiency state of the body
late start of treatment and poor sanitation of local forms of purulent-septic infection
violation of child care rules
violation of the rules of asepsis and antisepsis
chronic foci of maternal infection
Sepsis is classified according to the location of the primary focus:
pulmonary
intestinal
otogenic
umbilical
The following clinical forms of sepsis are distinguished:
Septicemia
Septicopyemia
Septicemia (septic shock) occurs due to the massive entry of pathogenic microorganisms into the bloodstream and is more common in premature infants.
Clinical manifestations:
severe intoxication
high fever
pale skin with a cyanotic tint
dyspeptic disorders
changes from the SSS
weight loss
septic hepatitis develops
The child dies from septic shock.
Septicopyemia is characterized by a wave-like course due to the constant development of new pyemic foci in the body. This form is more common in full-term babies.
Clinical manifestations:
severe intoxication
signs of respiratory failure
signs of CV insufficiency
development of new purulent foci (osteomyelitis, meningitis, otitis, paraproctitis, purulent pneumonia)
According to the duration of sepsis, there are:
acute course – from 3 to 6 weeks
subacute course – from 1.5 months to 3 months
prolonged course - more than 3 months.